Labour induction
Inducing labour means that the birth process is artificially initiated.
Inducing labour always takes place in a hospital under the supervision of a gynaecologist (a doctor specialised in female reproductive health).
This brochure provides general information about inducing labour. You can inquire about this procedure at the hospital where you’ll be giving birth.
Why induce labour?
Gynaecologists typically advise inducing labour if they expect that the situation will be better outside the uterus for the baby than it is inside.
Labour is induced when the baby is still in good condition and is expected to cope well with a normal delivery. Another reason to induce labour may be if you develop severe symptoms of your own. Common reasons for inducing labour include a pregnancy that is already or nearly overdue, waters that have been broken for more than 24 hours, high blood pressure, gestational diabetes or an oversized baby.
Overdue pregnancy
If you’re still pregnant one week after your due date, your pregnancy is considered ‘overdue’. At this point, you have been pregnant for 41 weeks. In this case, the gynaecologist always performs an ultrasound to check the amount of amniotic fluid.
A CTG (cardiotocogram) will also be performed to record the foetal heartbeat. If, according to these exams, the baby’s condition is deteriorating, the gynaecologist will advise inducing labour.
Waters have been broken for more than 24 hours
The first sign that a woman has gone into labour is often their water breaking. If the waters have been broken for more than 24 hours, this is referred to as pre-labour rupture of membranes. The labour process can still begin on its own.
However, childbirth in hospital is advised, as there is a greater chance of infection.
If your waters have been broken for a long time, you should check your temperature. In case of a fever (higher than 38°C), you should contact your midwife or gynaecologist.
If the waters have been broken for more than three days in a pregnancy at 37 weeks and 0 days, there is little chance that the contractions will begin spontaneously.
The gynaecologist usually recommends inducing labour between 24 hours and three days after the waters have broken.
If the waters break prior to 37 weeks, induction is often postponed as long as there is no sign of infection.
Undersized baby
If the midwife or gynaecologist believes that your baby’s too small, an ultrasound can be done to confirm this.
Regular ultrasound scans will provide information about your baby's growth. If necessary, an additional check of the child’s condition will be done with a CTG. If your baby shows insufficient growth or its condition threatens to deteriorate, the gynaecologist may advise inducing labour.
Deterioration of the placenta’s functioning
Your baby receives nutrients and oxygen via the placenta. In cases of high blood pressure, for example, or gestational diabetes, the placenta may not function properly.
The gynaecologist may decide to induce labour if it is apparent that it would be better for the child.
Other reasons
There are many reasons for inducing labour. These may relate to the course of the woman's previous delivery or with other problems with the current pregnancy. At some hospitals, including VieCuri, a woman may arrange to have labour induced without a medical reason for doing so.
Gynaecologists sometimes differ in opinion about when labour induction is really necessary. Do you have doubts about whether it’s really necessary to induce labour in your case? Discuss your concerns with your gynaecologist.
There may be another viable option, like keeping a close eye on the baby or mother while waiting for the labour to begin by itself.
If you and your gynaecologist cannot come to an agreement, you can always speak to another gynaecologist or seek a second opinion at another hospital.
Preparation
To determine whether labour may be induced, the gynaecologist will perform an internal examination, which is usually completed on an outpatient basis.
What to bring
You’ll need to bring the same items as you would for a 'normal' delivery, such as clothing for during and after childbirth, toiletries and baby clothing. It’s also a good idea to bring anything that helps you relax and pass the time. You may not experience many contractions during your first few hours of labour. In which case, it’s nice to have ways to distract yourself. You can use our wi-fi network.
Cervical ripeness
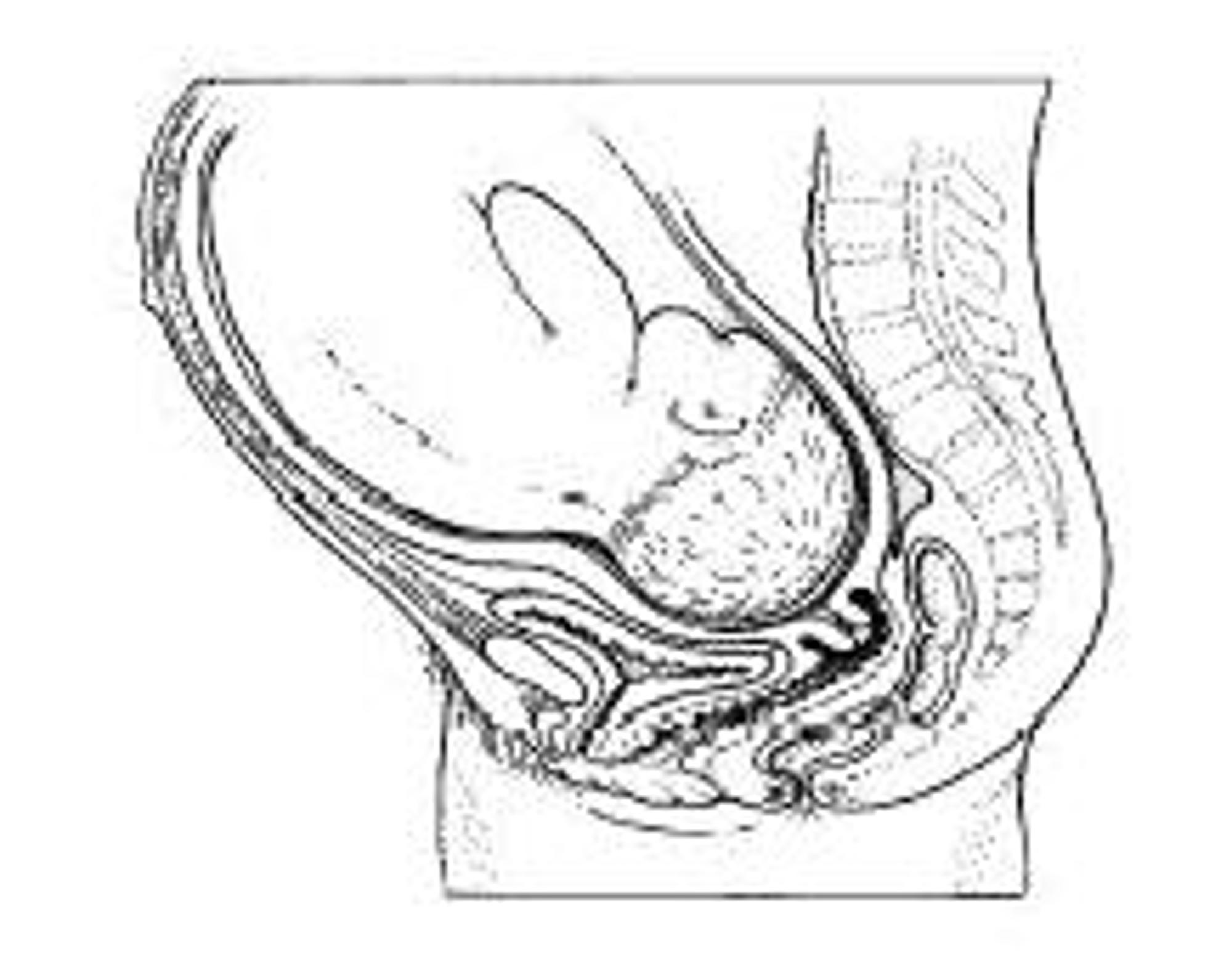
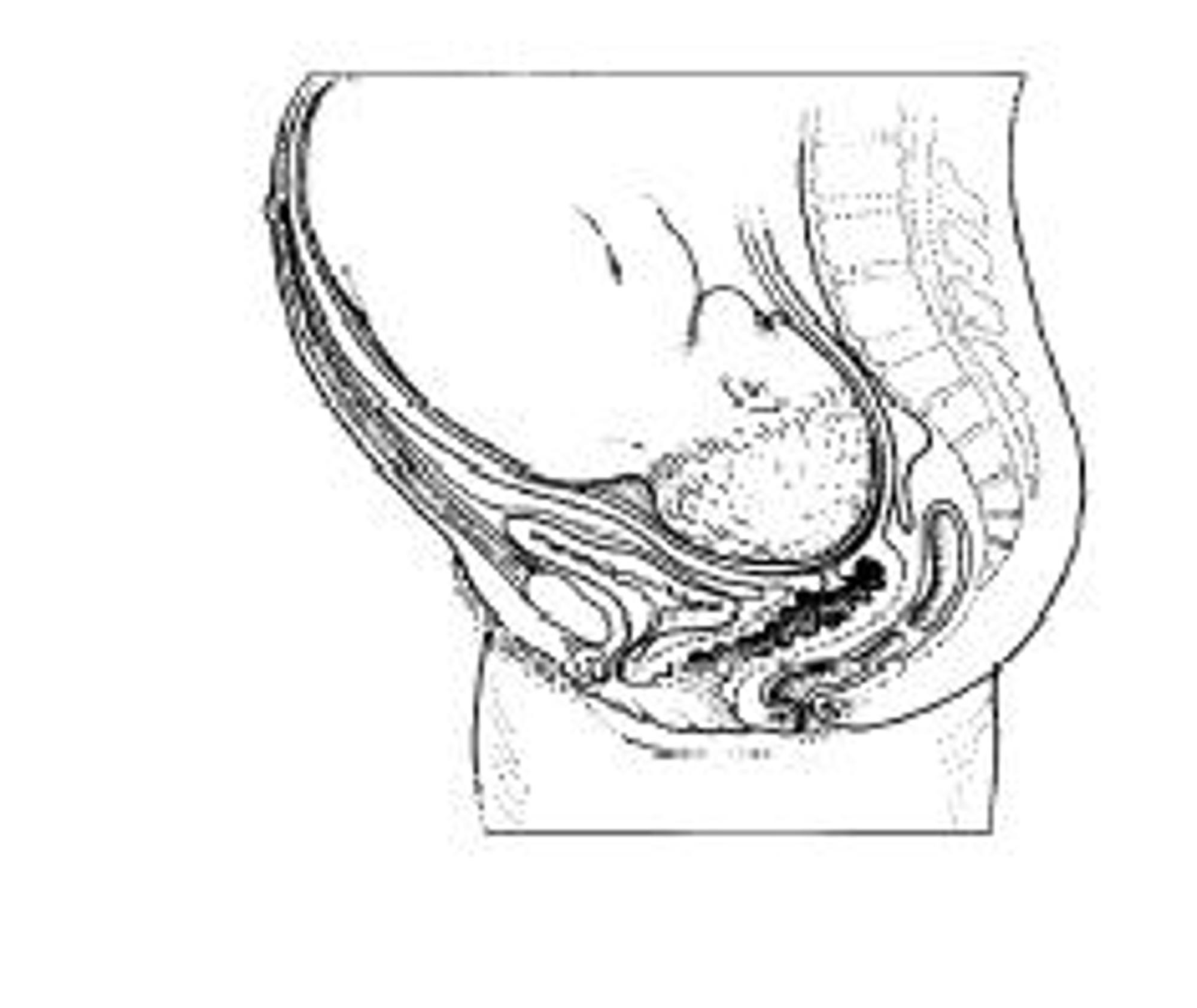
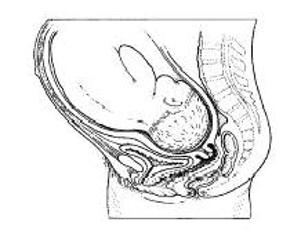
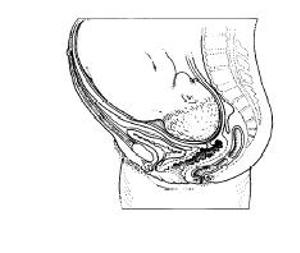
Midwives and gynaecologists describe the condition of the cervix according to its ‘ripeness’.
An ‘unripe’ cervix is still long and firm.
This is called a 'closed portio' ('portio vaginalis' is the medical term for the visible portion of the cervix). Usually, the cervix is not dilated yet.
A ripe cervix is typically shorter, which is referred to as an ‘open portio’.
An open cervix feels softer and has often begun to dilate.
In case of an unripe cervix
If the cervix is unripe, but there’s a compelling reason to induce labour, the gynaecologist may advise 'ripening' the cervix. In medical terms, this is known as ‘priming’ (preparing) the cervix.
The following drawings illustrate a ripe and an unripe cervix.
Cervical ‘ripening’ methods
Prostaglandins are hormones that promote cervical ripening. These hormones help stimulate labour .
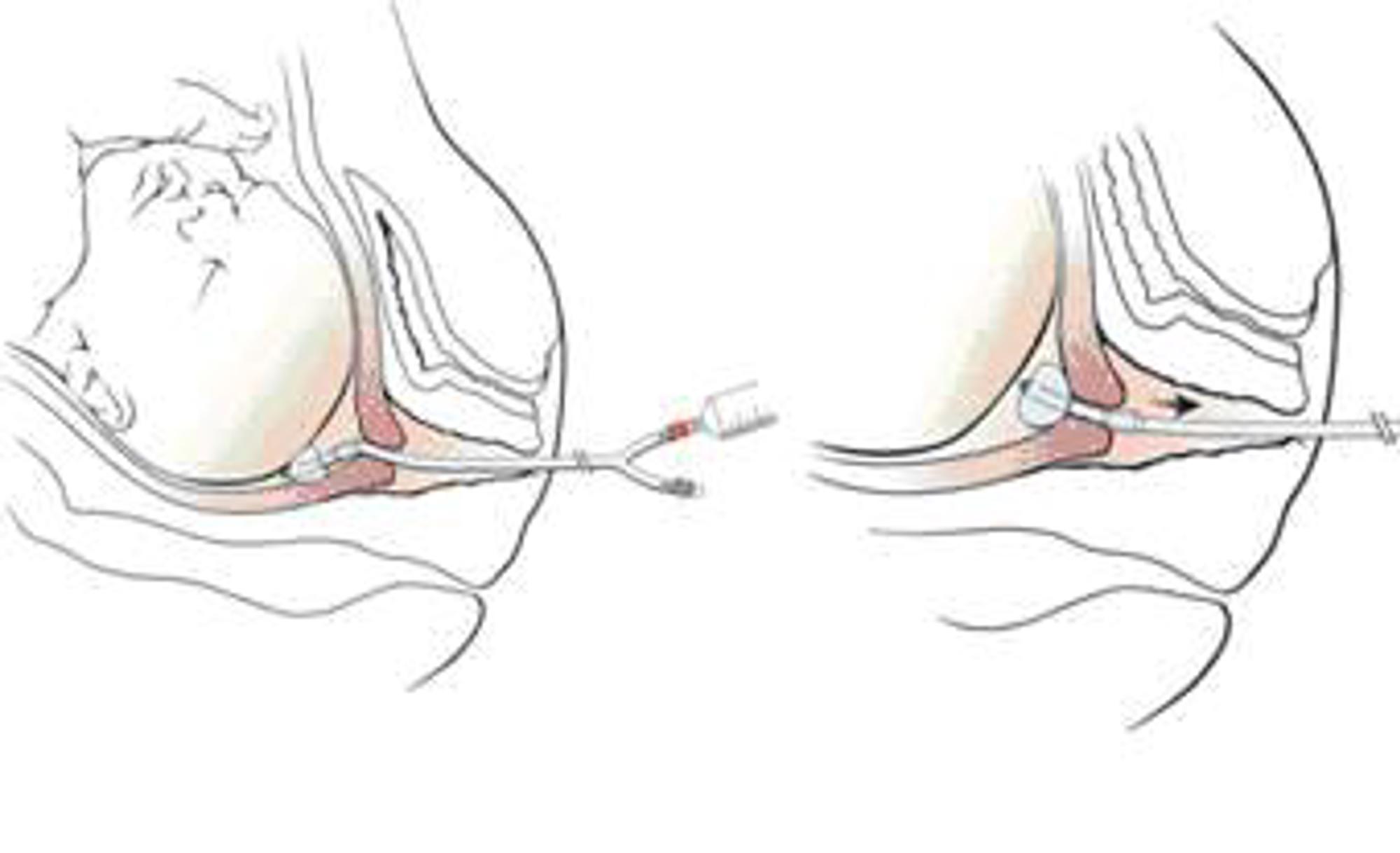
Balloon catheter insertion
One way to ripen the cervix is to fit a (Foley’s) balloon catheter. The catheter’s balloon exerts pressure, which causes prostaglandins to release naturally.
We begin by performing a CTG exam to check the status of your baby. The catheter is inserted in the ultrasound room via a speculum, while you lie in the leg rests or in a gynaecological chair. The speculum is an instrument that can be used to open the vagina.
The doctor or midwife inserts the balloon past the inner cervical opening. The balloon is then filled with water, causing you to feel a pressure at the bottom of your abdomen. The catheter is kept under tension by fastening it to your leg with a plaster.
Once the balloon is (properly) fitted, you’ll lie back in a normal position in bed during a CTG exam. In some cases, patients may go home with the balloon fitted in place. However, this will entail performing CTG exams twice daily: in the morning and in the evening.

You may already be having some uterine contractions, which can promote the ripening of the cervix.
After 12-24 hours, the cervical ripeness will be assessed. Taking into consideration how ripe the cervix is, the care professionals will discuss how to proceed. Reinsertion of a balloon catheter is also possible (no more than 48 hours total). After the balloon catheter is fitted, you may experience some blood loss. But there is no call for alarm.
Use of misoprostol (prostaglandine-E1)
Misoprostol tablets are another method for inducing labour. These tablets can be administered while the balloon is still in the uterus.
These tablets can be swallowed (orally) or inserted vaginally during an internal examination (using two fingers in the vagina to feel the ripeness of the cervix).
On the first day, the doctor will usually recommend swallowing the tablets. If a second day of misoprostol is required, the doctor will usually recommend that it be inserted vaginally. Misoprostol may be administered no more than three times within a 24-hour period. You will not be allowed to go home if this induction method is applied.
After prostaglandins are inserted, a care technician will perform a CTG exam to check the status of your baby. Particularly in case of a very unripe cervix, it will be necessary to repeat the treatment for a few days.
Prostaglandins not only ripen the cervix, they also stimulate contractions. Women often develop the condition known as ‘hard bellies’ after prostaglandins have been administered. This condition does not mean that there are any contractions yet. We only speak of contractions once the cervix is dilated. Sometimes, the ‘hard bellies’ do turn into contractions and labour begins.
Inducing labour
Labour induction involves initiating contractions and monitoring the condition of your baby.
Artificially breaking waters
The waters are broken during a vaginal examination. Your baby will not notice a thing from this process. Once your waters have been broken, you’ll feel warm amniotic fluid flowing through your vagina.
Stimulating contractions
Contractions are often stimulated by means of an IV drip. A needle is inserted into a blood vessel in your hand or forearm and connected to a thin, flexible tube.
A pump delivers medication (oxytocin) via the IV drip to trigger contractions. The dose increases gradually. Subsequently, the contractions begin slowly.
Another way to stimulate contractions is to either swallow or vaginally insert prostaglandin tablets. This is done in the same way as described for ripening the cervix.
Monitoring the baby and the contractions
Your baby's well-being will be monitored via a CTG exam. This exam can be performed externally, via an elastic strap that encircles the mother’s abdomen. Typically, however, the CTG is performed internally by fastening a thin wire (a foetal scalp electrode) to the baby’s scalp to record the foetal heartbeat.
The contractions are recorded via a strap around the abdomen. The contractions and foetal heartbeat are recorded wirelessly, which allows free movement around the birthing suite.
How does the childbirth proceed further?
Once labour has been induced, the birthing process usually proceeds like a ‘normal’ delivery. The contractions gradually grow more regular, intense and painful until you’re fully dilated (i.e. the cervix reaches 10cm).
You’re usually free to handle contractions in your own way, such as sitting in a chair, standing next to the bed, by lying down or sitting up in bed, in the bath or in the shower or sitting on a Skippy ball. The expulsion (the pushing) and the birth of the baby and placenta are no different from a ‘normal’ delivery. In general, the birth takes place within a 24-hour period. The riper the cervix, often the faster the dilation. Usually the birth of a second or subsequent child is faster than that of a first one.
With an induction via prostaglandins, you will often develop a very hard, painful stomach without actually having contractions yet. If your contractions are too painful and your cervix has begun dilating, you can request pain relief. In which case, you may be administered a strong analgesic agent (remifentanil) via an IV drip. Another option for pain relief is an epidural (epidural anaesthesia).
Post childbirth
Once your baby is delivered, the doctor or midwife will perform a check-up. If there’s cause to do so , the paediatrician will perform this examination. If all goes well, you’ll be able to go home within a few hours.
You may be advised to stay in hospital longer if, for example, your waters were broken for over 24 hours or in cases of gestational diabetes. If you baby is born underweight or prematurely, your hospital admission may last longer. You may remain with your baby if the child has been admitted to the incubator suite. In some cases, your own health may be a reason for you to stay longer. For example, in the case of high blood pressure or significant blood loss that requires a blood transfusion. You can remain with your baby if both of you can still receive the proper treatment.
Who will be present at the delivery?
Because medical criteria have to be observed for inducing labour, you’ll receive a medical referral to give birth in hospital. Sometimes, the gynaecologist supervises the delivery of your baby. In other situations, this will be done by a midwife or a doctor working
under the supervision of the gynaecologist who is available for them to consult.
In addition, nurses, trainee nurses and midwives and even co-assistants (medical students) may also be present. You can inquire in advance about who will be attending your delivery. You can record your wishes in a birth plan.
Risks and complications
Issues or complications can arise with any delivery, whether or not labour is induced. A few complications that could be connected to induced labour are mentioned below.
Prolonged labour
If labour is induced before the cervix has ripened properly, there is a greater chance of a prolonged labour. Sometimes, the cervix does not dilate fully and a Caesarean section is required.
Prolapsed umbilical cord
When the mother’s waters break, the umbilical cord may slip down alongside the baby’s head if it has not descended properly, or along the coccyx in a breech birth presentation. In such a case, a Caesarian section will be necessary.
Uterine hyperstimulation
Hyperstimulation refers to when too many contractions come on too close together. If this lasts for an extended period, the unborn baby may become oxygen deprived. Hyperstimulation is usually remedied by lowering the position of the IV pump. It may be necessary to administer medication to slow down the contractions, and this allows them to return to a normal pace.
Uterine infection
If the waters have been broken for a long time, the mother runs a slightly higher risk of developing a uterine infection either during or after labour. In fact, this complication in not a result of the induction itself, but is related to the reason for inducing labour.
Inflammation of the baby’s head or buttocks
As previously described, a thin wire (the scalp electrode) is fastened onto the baby's scalp to record the foetal heartbeat. For babies lying bottom or feet first in-utero (i.e. breech position), this wire is attached to their buttocks. In rare instances, babies can develop an infection where the electrode was attached. This is not serious, but it is uncomfortable for the child.
Improperly positioned IV drip
The exertions of childbirth may cause the IV needle to dislodge entirely or become improperly positioned.
Though this is not a big deal, women often do not appreciate having another needle inserted into their hand or arm.
Labour is most often induced without any complications. The risks of induced labour are usually no greater than those of a normal birthing process. It is imperative, however, that labour be induced under proper supervision and guidance.
There are many stories circulating about how induced labour is more painful than normal labour. This is difficult to prove because no two deliveries are the same.
Can mothers do anything to induce their own labour?
Women commonly ask whether there’s anything they can do to induce their own labour. Unfortunately, this is not so easy. Although some recommend using a 'miracle’ oil, its benefits have never been proven. It can, however, cause annoying intestinal cramps.
Membrane stripping
Another method for initiating labour naturally, without inducing it, is membrane stripping. During an internal examination, the midwife inserts fingers into the cervix to separate the amniotic membranes from the uterus. This process can be painful,
and it often results in blood loss. This is in no way harmful to you. Membrane stripping is not very effective when the cervix is unripe. The chances of a spontaneous childbirth afterwards are small.
Appointments at VieCuri Medical Centre
When the gynaecologist schedules your labour induction with you, he or she cannot say anything about how busy the birthing suites are. If there’s no room on the delivery suite on the scheduled morning or evening, the labour induction may be moved to later in the day or to a subsequent one.
Be sure to call the birthing suites at 7.00am on the day your labour will be induced, and at 8.00am or 7.30pm in case you’ll undergo balloon induction.

Bring your hospital card and a valid ID
The day that your labour is induced is not necessarily the same day that your baby will be delivered. The induction may not be effective immediately; sometimes, the body is not ready to give birth. It sometimes takes time and patience to induce labour. Bear in mind that we may allow you to return home. In which case, we’ll schedule a follow-up appointment with you.
Additional information
For additional information and to consult educational videos, see the following websites:
Questions
If you have questions after reading this information, please make your inquiries during your next visit to your midwife or gynaecologist.
Pressing and urgent questions
If your labour has started or you have a question about your pregnancy that cannot wait (i.e. an emergency), you can call, day or night, your midwife or the Delivery Ward of the Birthing Centre.

Vragen
Heeft u na het lezen van deze informatie nog vragen? Stel uw vragen tijdens het eerstvolgende bezoek of bel naar:
Contact
Opmerkingen
Ziet u een typfout, een taalkundige fout, of heeft u moeite met de leesbaarheid?
Ziet u teksten of afbeeldingen met auteursrechten die wij niet hebben vermeld?
Stuur een e-mail naar communicatie@viecuri.nl en we zoeken een passende oplossing.
Disclaimer
Deze informatie is algemeen en geen behandeladvies. De informatie is ook geen vervanging van de afspraken die tussen patiënt en zorgverlener zijn gemaakt. VieCuri kan niet aansprakelijk worden gesteld voor schade als gevolg van mogelijke onjuistheden. Bekijk hier de uitgebreide disclaimer.